Overview
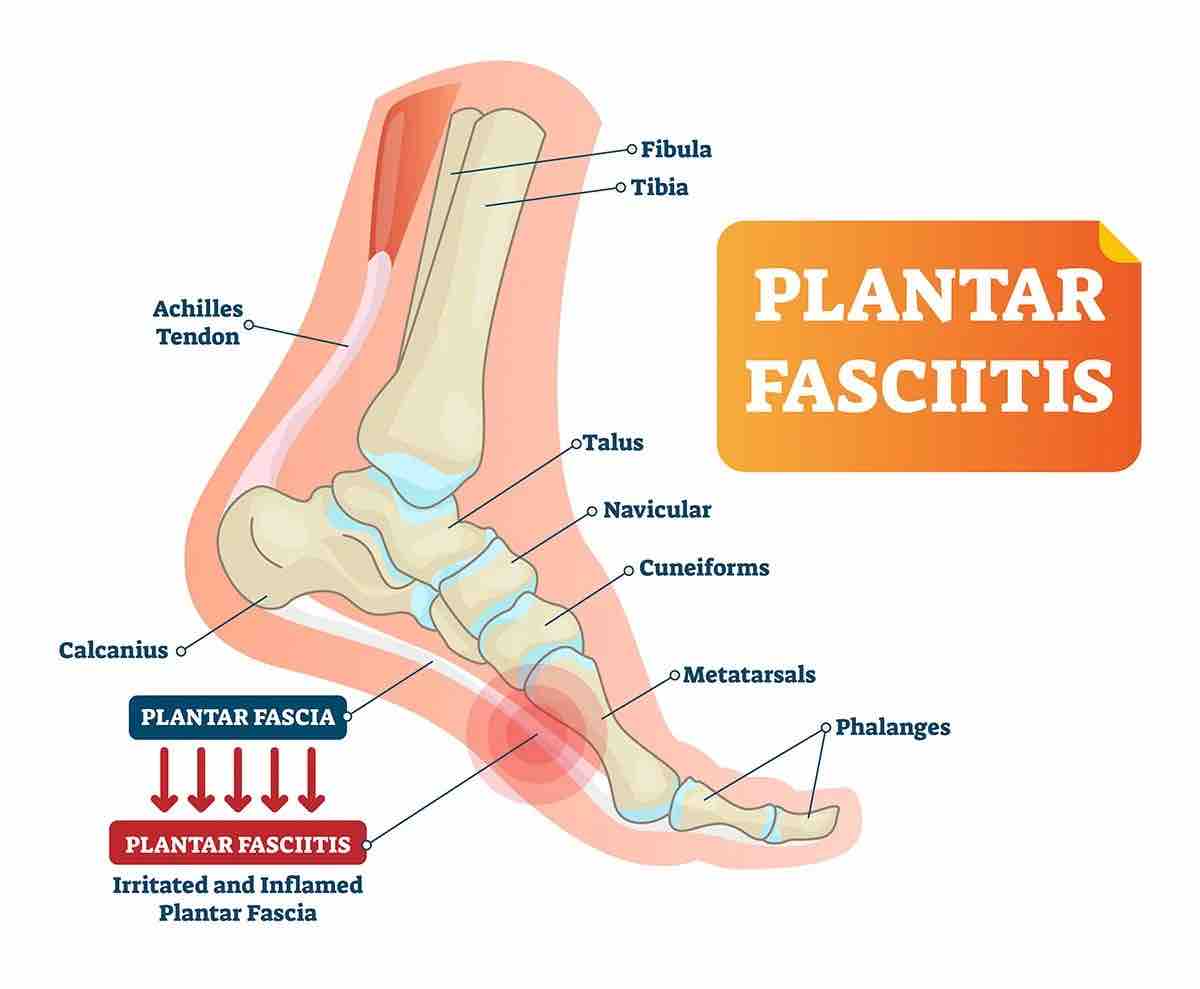
Plantar Fasciitis is one of the most common causes of heel pain, resulting from inflammation of the plantar fascia, a thick band of tissue connecting the heel to the toes. This condition often leads to stabbing pain, especially with the first steps in the morning or after long periods of standing or sitting.
The plantar fascia helps support the foot’s arch, and when overused or overstretched, it can become damaged and inflamed, causing discomfort. This condition is prevalent in runners, individuals who are overweight, and those with flat feet.
Treatment often involves rest, icing, over-the-counter medications, and stretching exercises to alleviate pain and inflammation. While most cases can be managed at home, persistent pain may require professional medical evaluation.
What is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain, resulting from inflammation of the plantar fascia — a thick, fibrous band of tissue that runs along the sole of the foot, connecting the heel bone (calcaneus) to the base of the toes. This tissue supports the foot’s arch and plays a crucial role in normal foot mechanics during walking or running.
When the plantar fascia is overused or overstretched, often from activities like standing, walking, or running, it can lose its elasticity and become irritated, leading to inflammation. This inflammation causes pain, particularly during the first steps in the morning or after prolonged periods of standing or sitting. While plantar fasciitis commonly affects one foot, it can sometimes impact both.
If heel or foot pain persists for more than a week, it’s important to consult a healthcare provider for evaluation and treatment.
Symptoms
What are the Symptoms of Plantar Fasciitis?
The most common symptoms of plantar fasciitis include:
- Heel pain.
- Pain in the arch of your foot.
- Stiffness, especially in the morning or after periods of inactivity.
- Swelling around the heel.
- A tight Achilles tendon.
What Does Plantar Fasciitis Feel Like?
People with plantar fasciitis typically experience an achy or sharp pain in the heel or along the bottom of the foot. The pain can vary depending on the time of day or activity level. Some common sensations include:
- Morning Pain: Sharp or stabbing pain when standing up after sleeping or sitting. It often improves after walking for a few minutes.
- Dull Ache: A constant, dull pain that may persist throughout the day.
- Pain After Activity: Although exercise or movement may temporarily relieve pain, it usually worsens after you stop.
- Heel Stiffness: Climbing stairs or walking long distances can be difficult due to stiffness.
- Burning Sensation: Some may feel a burning pain radiating from the heel.
The discomfort usually develops gradually and is often worse in the morning or after periods of rest. Overactivity can exacerbate the condition, leading to increased pain after stopping the activity rather than during it.
What Causes Plantar Fasciitis and Who is at Risk?
Plantar fasciitis is primarily caused by overstretching or overuse of the plantar fascia, the ligament that connects your heel to your toes. Small tears in the fascia tissue can also lead to inflammation and pain. While doctors once believed heel spurs caused plantar fasciitis, this is no longer considered the primary cause.
Common causes and risk factors include:
- Age: Most common in individuals aged 40 to 70.
- Foot Structure: Flat feet or high arches increase the risk.
- Physical Activity: Activities like running, walking, standing for long periods, or playing sports can strain the plantar fascia, especially on hard surfaces.
- Weight: Obesity or rapid weight gain can place additional stress on the foot.
- Footwear: Shoes with poor cushioning or support, such as flat shoes or flip-flops, can exacerbate the condition.
- Pregnancy: Women, particularly during late pregnancy, may develop plantar fasciitis due to added weight and changes in foot mechanics.
In addition, those who work on hard surfaces without proper footwear or exercise without stretching may also be more prone to developing plantar fasciitis.
How is Plantar Fasciitis Treated?
Plantar fasciitis can often be managed effectively with a combination of home treatments and medical interventions. Here are the most common approaches:
Home Treatments:
- Rest: Limit activities that strain the foot, such as running or standing for extended periods.
- Icing:Apply ice to the affected area for 10 to 15 minutes, twice a day, to reduce inflammation.
- Supportive Footwear: Wear shoes with good arch support and cushioning, avoiding flat shoes or sandals.
- Over-the-Counter (OTC) Pain Relief: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or aspirin can reduce pain and swelling.
Stretching and Physical Therapy:
- Stretching Exercises: Gentle stretches targeting the calves and plantar fascia can improve flexibility and reduce pain. A physical therapist can guide you through these exercises to strengthen lower leg muscles and support your foot’s structure.
- Night Splints: These braces hold the foot in a stretched position overnight, reducing morning pain.
- Orthotics: Shoe inserts provide additional arch support and help distribute pressure across the foot.
Medical Interventions:
- Corticosteroid Injections: These anti-inflammatory medications can be injected directly into the plantar fascia to reduce severe pain and swelling. Sometimes, ultrasound guidance is used to ensure accuracy.
- Shockwave Therapy: Extracorporeal shock wave therapy uses sound waves to stimulate healing in the plantar fascia. While side effects can include bruising or swelling, this therapy can be effective when other treatments don’t work.
Surgical Options:
Surgery is a last resort, generally only considered if the pain persists for more than 6 to 12 months despite other treatments. Surgical options include:
- Gastrocnemius Recession: Lengthening the calf muscle to reduce strain on the plantar fascia.
- Plantar Fascia Release: Partially cutting the plantar fascia ligament to relieve tension and inflammation.
By following these treatments, most people find relief from plantar fasciitis without needing surgery.
Conclusion:
Plantar fasciitis can be a challenging condition, but with the right treatment approach, including physiotherapy and osteopathy, individuals can experience relief from their symptoms and regain mobility. If you suspect you have plantar fasciitis, consult a healthcare professional for an accurate diagnosis and a personalized treatment plan.