Muscular Dystrophy: Causes andTreatments
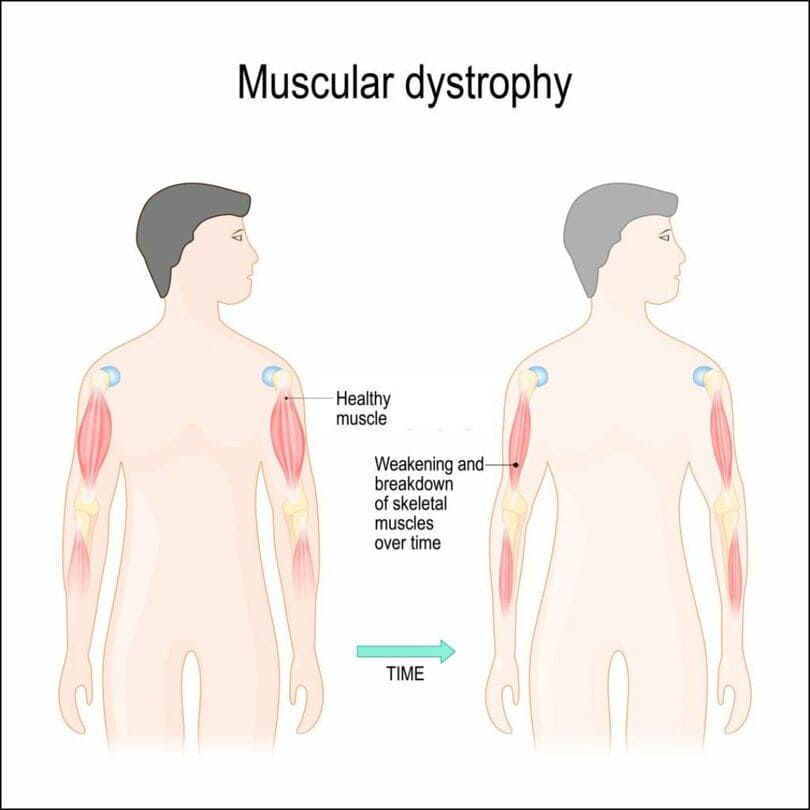
Introduction Muscular dystrophy is a group of genetic disorders characterized by progressive muscle degeneration and weakness. The condition stems from mutations in the genes responsible for the production of specific muscle proteins, leading to the gradual deterioration of muscle mass and function over time. While various types of muscular dystrophy exist, the most common forms typically manifest during childhood, predominantly in boys. However, certain variations might not become evident until adulthood. Symptoms The primary indicator of muscular dystrophy is the gradual weakening of muscles. Different signs and symptoms arise at varying ages and in diverse muscle groups, depending on the specific type of muscular dystrophy. Duchenne Type Muscular Dystrophy: Frequent falls Difficulty in rising from a lying or sitting position Challenges with running and jumping Waddling gait Walking on the toes Enlarged calf muscles Muscle pain and stiffness Learning disabilities Delayed growth Becker Muscular Dystrophy: Symptoms resembling Duchenne Muscular Dystrophy, albeit milder and slower in progression. Causes Muscular dystrophy originates from genetic mutations that impair the production of essential muscle proteins, resulting in the degeneration and weakening of muscle tissues. These mutations can be inherited or arise spontaneously, contributing to the development of specific forms of the disease. Understanding the underlying genetic mechanisms responsible for each type of muscular dystrophy is crucial for accurate diagnosis and targeted treatment approaches. Types of muscular dystrophy Duchenne Type Muscular Dystrophy: Duchenne muscular dystrophy is the most prevalent form of the condition, primarily affecting boys. This type typically manifests in early childhood and is characterized by progressive muscle weakness and wasting, leading to difficulties with mobility and motor functions. Common symptoms include frequent falls, trouble rising from a sitting or lying position, a waddling gait, and enlarged calf muscles. As the disease advances, it can also result in learning disabilities and delayed growth, significantly impacting the overall quality of life for affected individuals. Becker Muscular Dystrophy: Becker muscular dystrophy shares similarities with Duchenne muscular dystrophy, although the progression is generally slower and the symptoms milder. This type of muscular dystrophy often presents in the teenage years or even in adulthood, with manifestations such as muscle weakness, difficulties with movement, and potential complications related to mobility and muscle function. While it bears resemblance to Duchenne muscular dystrophy, the milder progression often allows for a more extended period of preserved mobility and functionality. Myotonic Dystrophy: Myotonic dystrophy is characterized by the inability of muscles to relax following contractions. This type typically affects facial and neck muscles initially, resulting in distinct physical features such as a long, thin face, drooping eyelids, and a swan-like neck. Apart from the facial and neck muscles, myotonic dystrophy can also involve other muscle groups, leading to a range of symptoms including muscle weakness, myotonia (prolonged muscle contractions), and potential complications affecting mobility and muscle function. Facioscapulohumeral Muscular Dystrophy (FSHD): Facioscapulohumeral muscular dystrophy primarily affects the face, shoulder, and hip muscles, often leading to the appearance of winged shoulder blades when the arms are raised. Onset can occur during the teenage years or later in life, presenting with symptoms such as muscle weakness, difficulties with movement, and progressive impairment of mobility. The variable age of onset and differing patterns of muscle involvement contribute to the diverse clinical presentation and progression of FSHD. Congenital Muscular Dystrophy: Congenital muscular dystrophy manifests early in life, either at birth or before the age of two, and can result in a range of outcomes depending on the specific form of the condition. Some variations progress gradually, leading to mild disabilities, while others can rapidly cause severe impairments. The symptoms may include muscle weakness, developmental delays, joint deformities, and potential complications related to mobility and motor functions, necessitating comprehensive management and support from an early age. Limb-Girdle Muscular Dystrophy: Limb-girdle muscular dystrophy affects the muscles around the hips and shoulders, resulting in difficulties with lifting the front part of the foot and frequent tripping. The onset of this type of muscular dystrophy typically occurs during childhood or the teenage years, leading to progressive muscle weakness, mobility challenges, and potential complications related to muscle function and overall physical activity. The diverse subtypes of limb-girdle muscular dystrophy contribute to the variability in the presentation and progression of the condition, necessitating tailored treatment approaches and comprehensive support for affected individuals. Clinic Services for Muscular Dystrophy: At York Rehab Clinic, our comprehensive range of services is tailored to effectively address the management of muscular dystrophy. With a focus on providing holistic and personalized care, our clinic combines various treatment modalities to support individuals with muscular dystrophy in their journey toward improved mobility and enhanced quality of life. Physiotherapy and Osteopathy: These services play a pivotal role in maintaining muscle strength, flexibility, and overall physical function. Through targeted exercises, manual therapy, and specialized techniques, our experienced physiotherapists and osteopaths work closely with patients to enhance muscle tone, improve joint mobility, and alleviate discomfort associated with muscular dystrophy. Shockwave Therapy: This innovative treatment option offered at York Rehab Clinic aids in promoting tissue regeneration and reducing pain through the application of focused shockwave energy. By stimulating the body’s natural healing mechanisms, shockwave therapy can effectively address muscle soreness and improve overall muscle function in individuals with muscular dystrophy. Knee and Spinal Decompression Therapy: Our clinic provides specialized decompression therapies, including knee and spinal decompression, to alleviate pressure on affected joints and spinal structures. By creating a controlled and gentle traction force, these therapies contribute to relieving pain and improving mobility, particularly in areas commonly affected by muscular dystrophy. Acupuncture: As an integral component of our treatment approach, acupuncture serves as a valuable complementary therapy in managing muscular dystrophy. By targeting specific acupoints, this technique can help reduce muscle tension, alleviate pain, and enhance overall well-being, promoting a comprehensive approach to managing the symptoms associated with the condition. PRP (Platelet-Rich Plasma) Therapy: At York Rehab Clinic, PRP therapy is utilized as an innovative regenerative treatment option to support muscle repair and enhance tissue healing. By harnessing the body’s