Anatomy of the facet joints
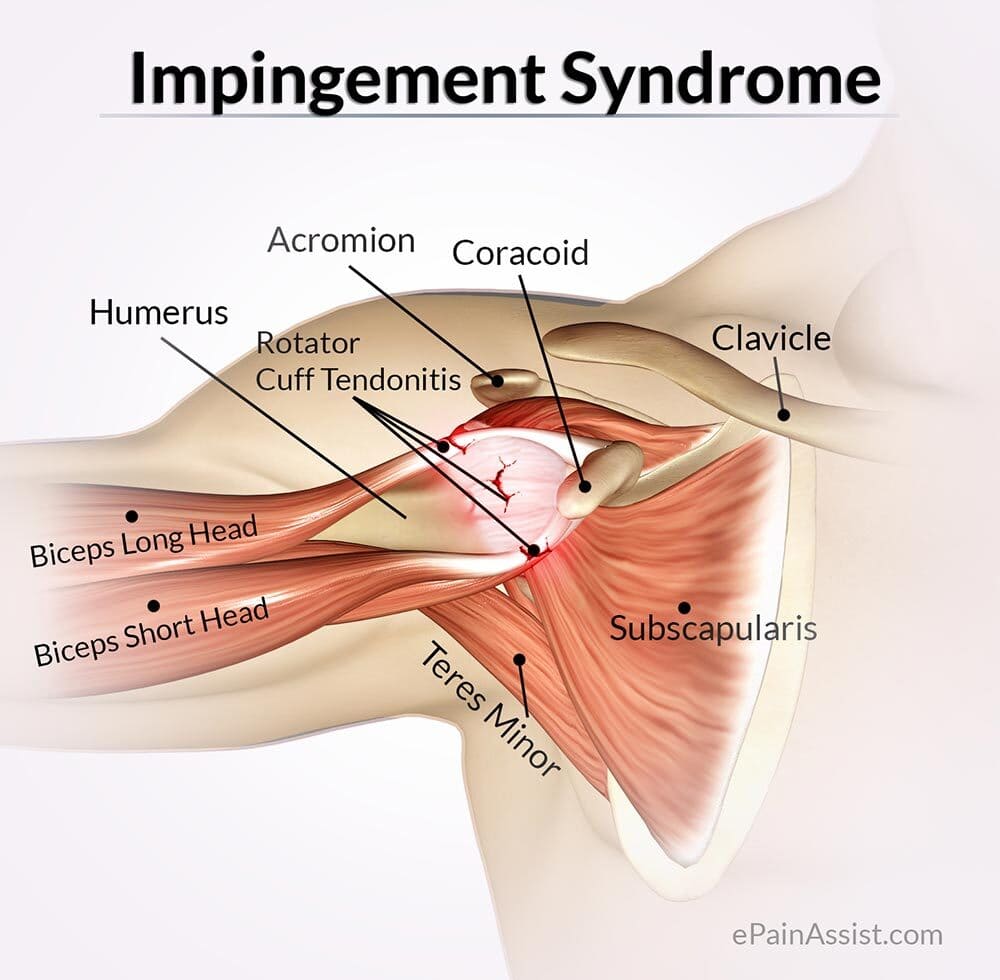
Facet Joint Syndrome is a condition in which arthritic change and inflammation occur, and the nerves to the facet joints convey severe and diffuse pain.
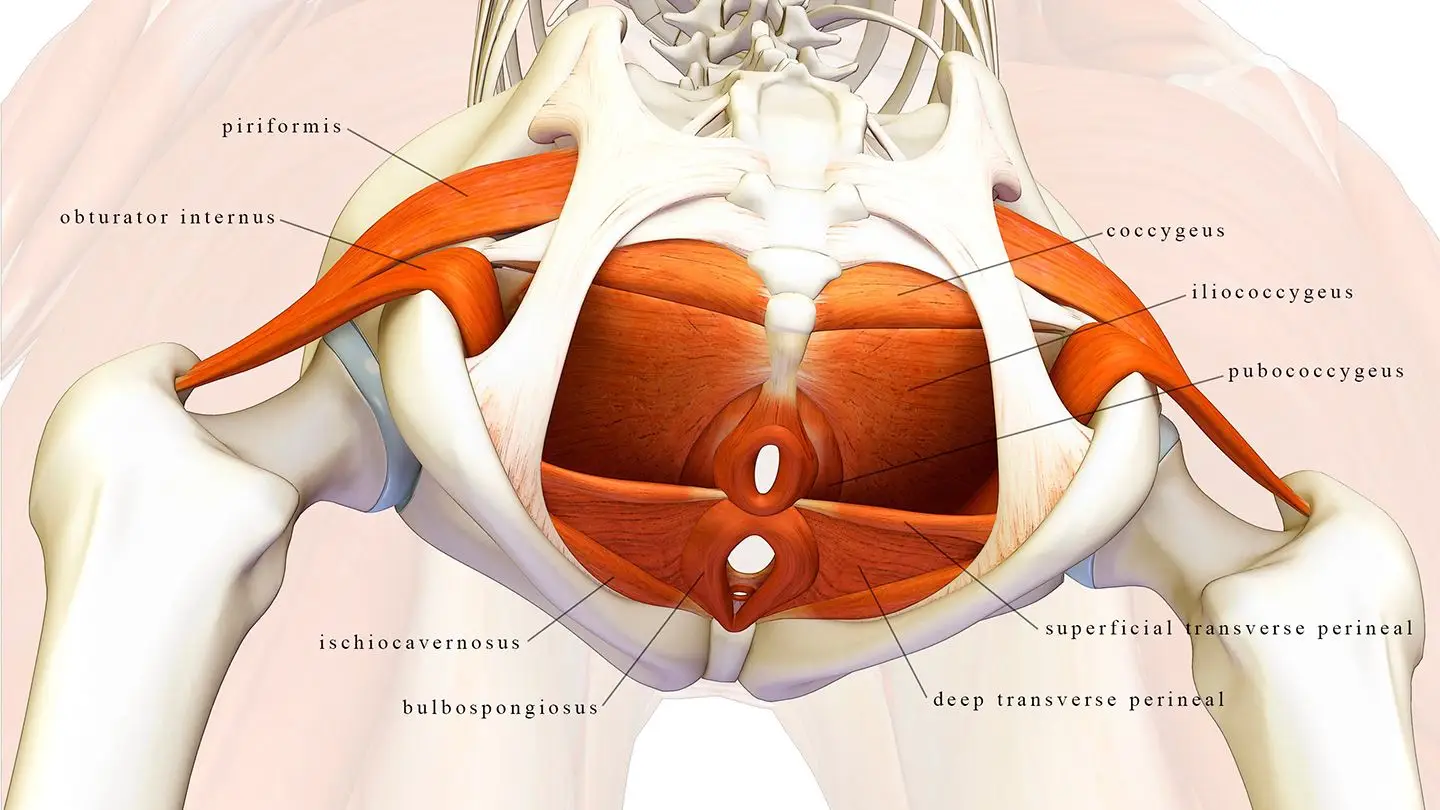
the facet joints are the connections between the bones of the spine. They allow the spine to bend and twist and they prevent excessive forward slipping or twisting. Like knee joints, they contain cartilage for smooth movement where two bones meet. The joints are lined with synovium and have lubricating joint fluid.
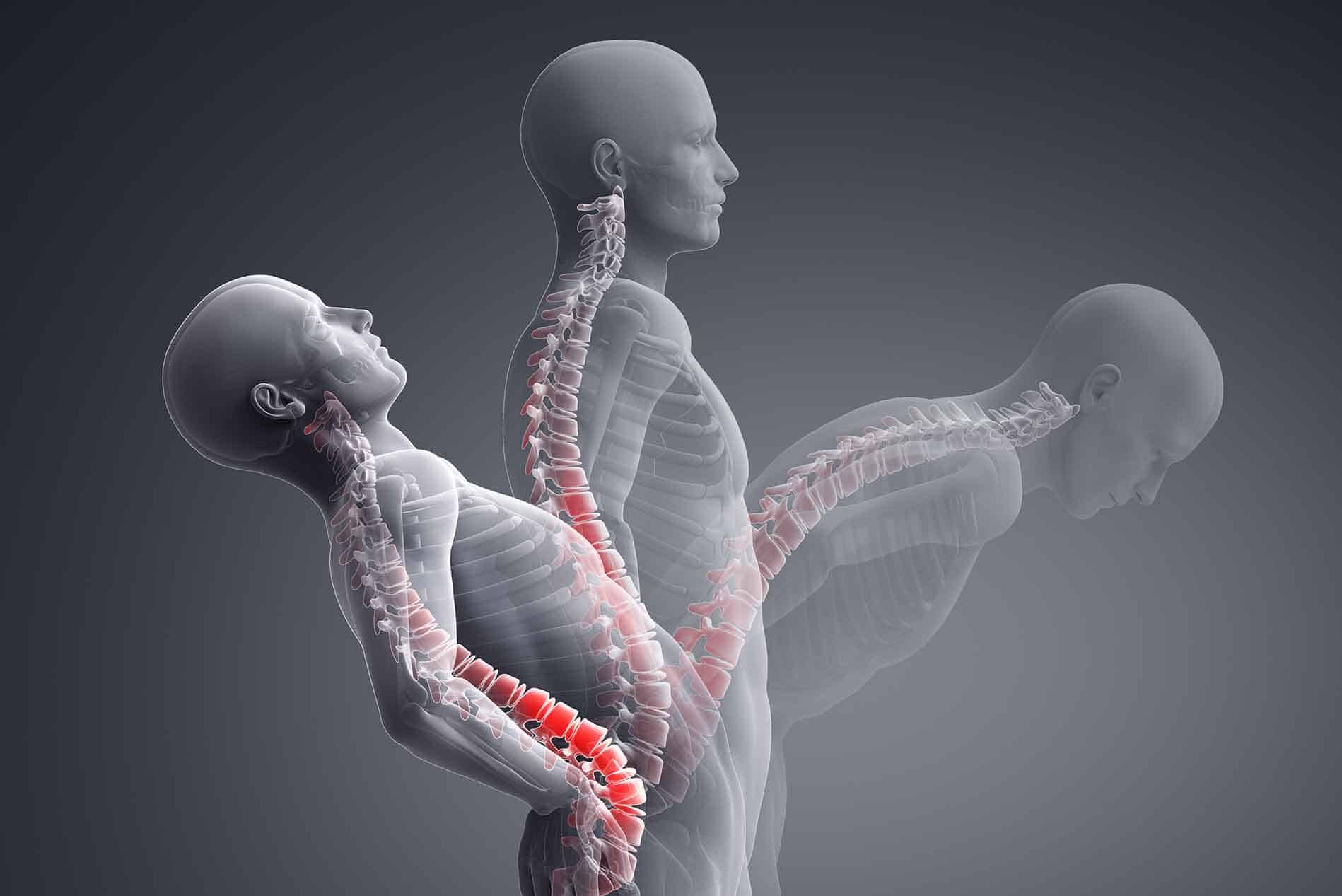
When these joints become inflamed due to injury or arthritis, they cause pain. If the affected joint is in the neck, it may lead to headaches and difficulty moving the head. If it is in the back, it may cause pain in the lower back, buttocks, or thighs.
The spine comprises movable bones called vertebrae, each of which functions as a three-joint complex with a large disc in the front and two facet joints in the back. This robust design keeps the bones linked together while allowing the spine to bend and twist. Facet joints are synovial joints that are lined with cartilage, lubricated with synovial fluid, and covered by a joint capsule. Healthy facet joints allow for smooth gliding and sliding movements in the back while preventing over-twisting.

What is facet joint syndrome?
Pain that comes from one or more facet joints is called facet joint syndrome or facet arthropathy. Degenerative changes in the spine may cause body weight to shift unevenly to the facet joints. This extra burden causes wear and tear on the joint and change it over time. The joint capsule thins, smooth cartilage breaks down and becomes irregular like a cobblestone street, and bone spurs may form. Similar to arthritis of the knee joint, these changes make it difficult for the joint to move fluidly and it reacts by becoming inflamed and irritated. The irritated joint sends pain signals to the brain via small nerves in the capsule called medial branch sensory nerves. In turn, the muscles in the area can stiffen and spasm.
In short, injury and degeneration cause the natural movement of these joints to break down, and the resulting inflammation, nerve irritation, and uneven pressure can cause intense pain and a significant decrease in your quality of life.
Common Signs and Symptoms of Facet Joint Pain
Facet joint pain can occur gradually, in the case of degeneration, or suddenly when caused by injury. The most common symptoms of Facet Joint Syndrome are:
- Difficulty twisting and bending the spine: These kinds of movements specifically exasperate the pain, which can make the activities of daily living difficult for you to perform.
- Pain and inflammation: The most commonly affected areas for pain and inflammation are your lower back and neck.
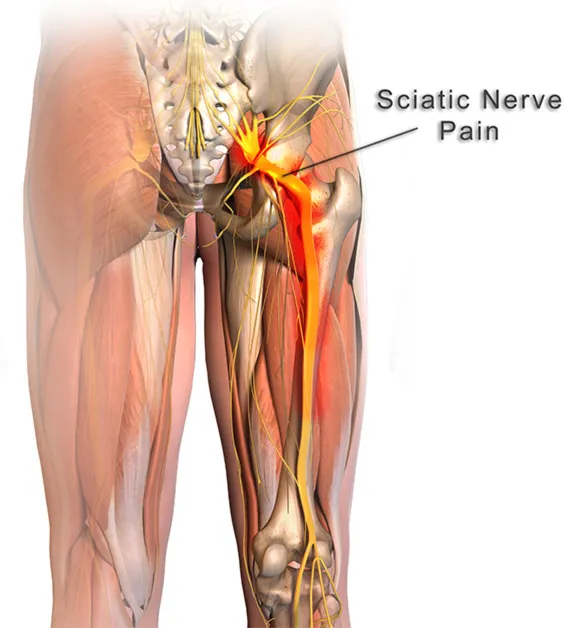
- Numbness, tingling, and muscle weakness: These occur when the edges of one of your facet joints rub on a nerve, which can also be very painful.
- Bone spurs: When your facet joints don’t line up correctly, your bones certainly will meet where they shouldn’t and rub against each other. Unsurprisingly, this also becomes very painful.
- Tenderness of certain areas of the spine: Occurs in response to inflammation in the nerves and muscles surrounding your facet joints.
These symptoms affect different parts of your body depending on which spinal nerves have been irritated.
- Neck pain and stiffness, such as might force you to turn your entire body to look at something, may indicate Cervical Facet Joint Syndrome.
- Pain near the middle of your back may indicate Thoracic Facet Joint Syndrome. Joint hypertrophy is less common in the thoracic spine due to the natural rigidity of the vertebrae.
- Low back pain and stiffness, such as might make it difficult to stand up from a chair or straighten your back, may indicate Lumbar Facet Joint Syndrome.
- Spinal stenosis can also occur in these areas, which narrows the spaces within your spine. This puts pressure on the nerves that travel through your spine to the rest of your body.
What are the causes?
As we get older, the cartilage in our joints wears down. An injury, repetitive movements, obesity, poor posture, and other spine conditions that change the way the facet joints align and move can cause pain.
Changes in the facet joints can begin with the deterioration of a vertebral disc. As the load of the body weight shifts to the facet joint, the cartilage breaks down, the joint space narrows, and the bones rub together.
Who is affected?
Facet joint syndrome occurs in both men and women. It is most common between the ages of 40 and 70 and in those prone to arthritis. It also may develop in people who’ve had a spine injury.
How does your osteopath diagnose a Facet Joint Injury?
The most accurate diagnosis of a facet joint injury is by palpation/touch. Osteopaths are trained to examine the spine, and they develop a remarkable sense of touch.
You may be asked to stand or move in different positions and point to where you feel pain. The osteopath may manipulate your joints or feel for tenderness over the spine.
Imaging studies, such as X-rays, CTs, or MRIs, may be ordered to help diagnose and check for other spine and hip-related problems, but some of the diagnostic tools you might expect a doctor to use are not needed in these cases. X-rays, MRI, and CT scans are useful to identify arthritic changes and fractures but are unable to detect a locked facet joint.
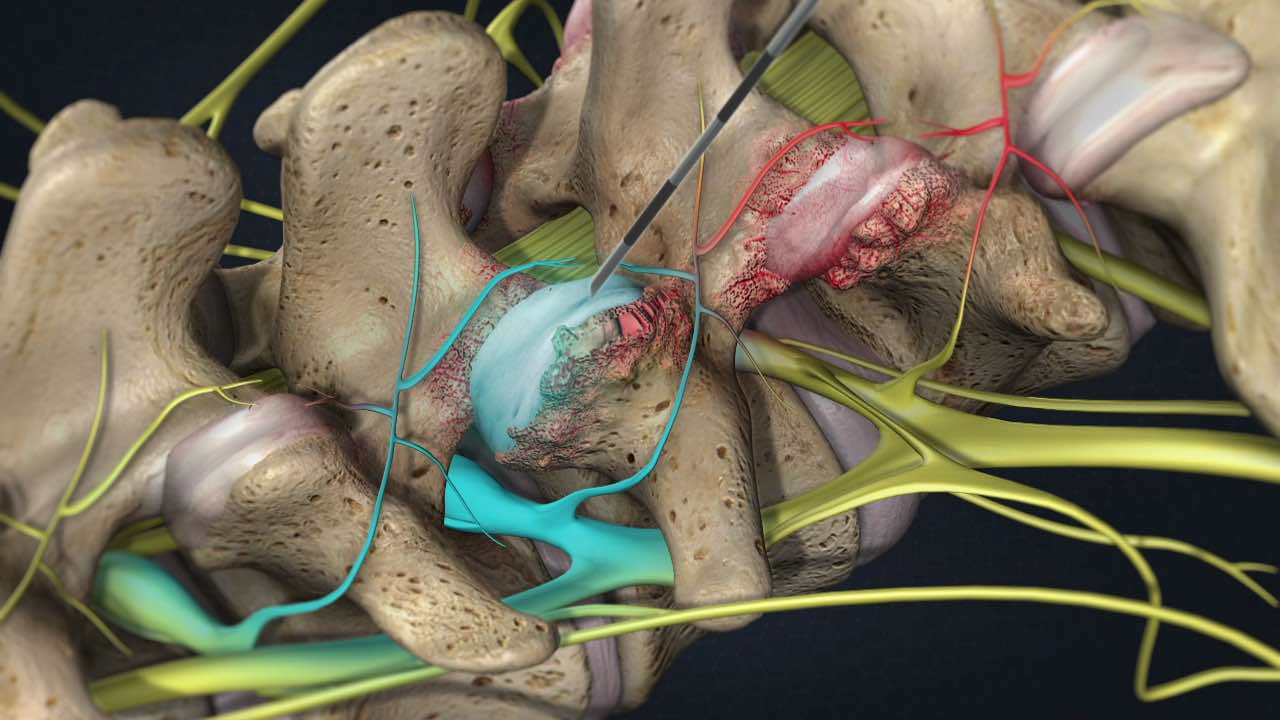
Facet Joint Injections can also be used to help identify facet joint pain. The facet joint is injected with a local anesthetic and corticosteroid medication. The injection is given using X-ray fluoroscopy to ensure accurate needle placement in the facet joint. Your pain level is evaluated before and 20-30 minutes after injection, and monitored over the next week. Facet joint involvement is confirmed if your pain level decreases by more than 75%. If your pain level does not change after the injection, it is unlikely that the facet joint is the cause of your pain.
Conservative Treatments for Facet Joint Pain
Pain from Facet Joint Syndrome can be treated conservatively with postural correction, physical therapy, massage, and chiropractic adjustment. These treatments can reestablish normal motion and increase the strength of the surrounding muscles to help support your spine. Conservative treatments are usually combined with anti-inflammatory medications and possibly muscle relaxers to diminish your acute pain while your body heals.
Most conservative treatments for facet syndrome involve postural correction, soft tissue massage, and manipulation of the affected areas.
Osteopathic clinicians and chiropractors are adept at restoring restricted and painful facet joints to move and can reestablish normal motion. Treatments are usually combined with a course of anti-inflammatory medications to decrease inflammation. Muscle relaxers may be used to decrease local muscle spasms.
In some cases, the pain may be so severe or the condition so advanced that conservative therapies are either too painful or otherwise ineffective. In these cases, a patient may be recommended for interventional pain therapy.
Minimally-Invasive Pain Therapy for Facet Joint Syndrome
If conservative treatments are ineffective or too painful, you may be recommended for one or more minimally-invasive surgical procedures. These procedures can be performed on an outpatient basis, and are done safely using fluoroscopic X-ray guidance. Interventional pain management therapies can offer rapid pain relief and help you resume normal activity.
Minimally-invasive treatment options may include:
- Facet Joint Injections: This procedure injects a corticosteroid into the affected joint which reduces pain and inflammation. These injections may also be used as part of the diagnostic process for additional treatments. Facet joint pain, but there is a limit on how frequently they can be administered.
- Facet Joint Block: This procedure is similar to a facet joint injection, but instead injects a local anesthetic into each side of the vertebrae. This will temporarily numb the pain and confirm the source of the injury.
- Radiofrequency Ablation: By destroying (ablating) the nerve endings surrounding the affected facet joint, pain signals can be blocked which will provide you with relief. This procedure often begins with a median nerve block to confirm the affected nerves for ablation.
How We Can Help
If you have questions about how York rehab clinic can help you get back to a life free from the pain of Facet Joint Syndrome. Our osteopaths and chiropractors specialize in conservative and none-invasive treatment plans for back, neck, and joint pain.
To book an appointment for Osteopathy, Chiropractic, and massage therapy in Richmond Hill, contact our professional team at York Rehab Clinic today at (416) 350-1940.