Overview
Achilles tendinitis is a common overuse injury affecting the Achilles tendon, which connects the calf muscles to the heel bone. This condition typically occurs due to repetitive stress on the tendon, particularly in athletes or individuals who engage in physical activities like running, jumping, or sudden increases in exercise intensity. Achilles tendinitis can also affect less active people, especially those with tight calf muscles or improper footwear.
Symptoms of Achilles tendinitis include pain, swelling, stiffness, and tenderness in the Achilles tendon, often worsening after physical activity. If left untreated, it can lead to more severe issues, such as an Achilles tendon rupture.
Treatment focuses on rest, physical therapy, and supportive footwear. Most cases can be managed with non-invasive treatments, but severe cases may require surgical intervention. Proper care and activity modification can prevent recurrence and ensure long-term tendon health.
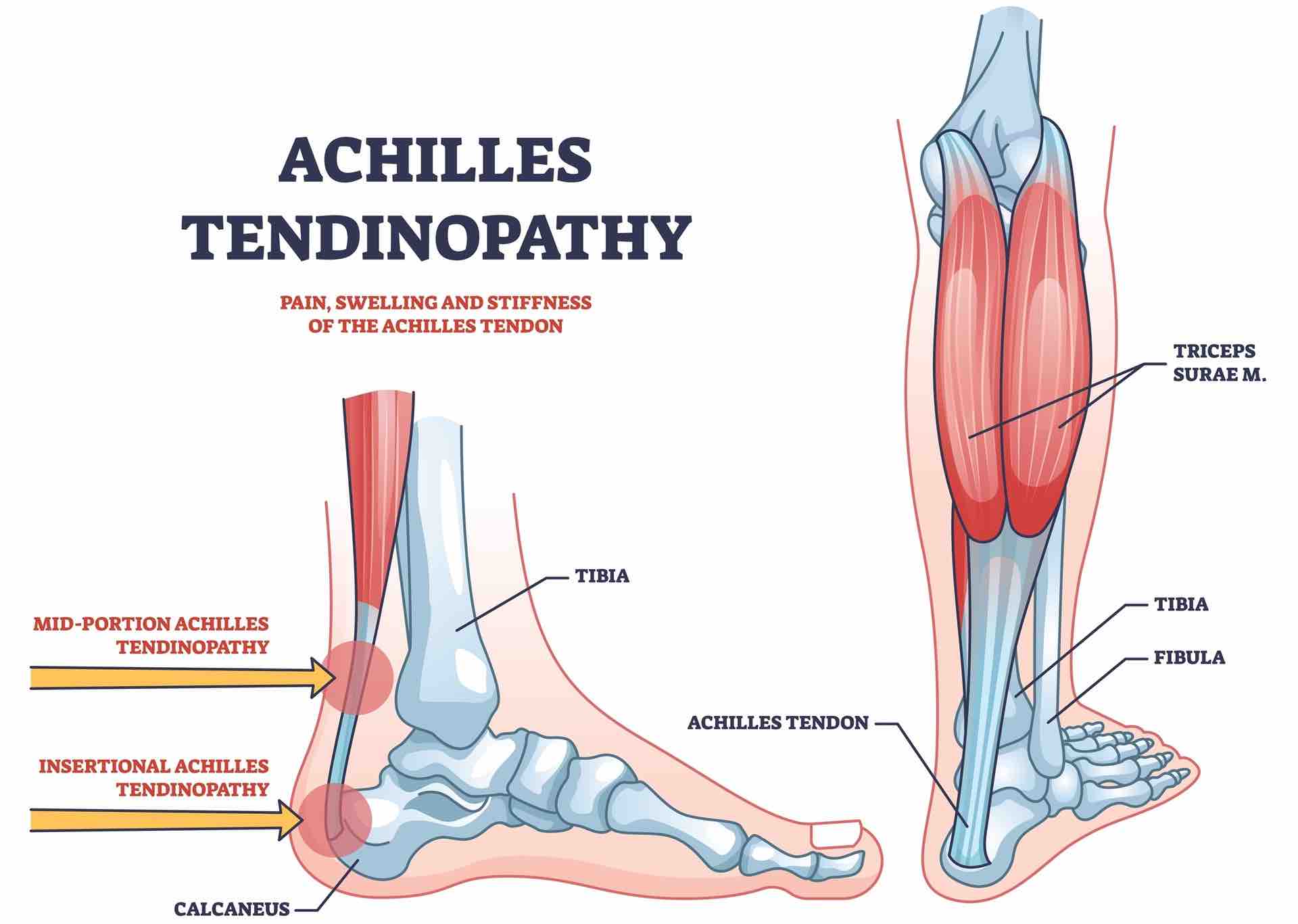
Types of Achilles Tendinitis
Achilles tendinitis can be classified into two types based on the location of the tendon affected:
- Noninsertional Achilles Tendinitis: This occurs when the fibers in the middle section of the tendon begin to break down, swell, and thicken. It typically affects more active individuals, such as athletes.
- Insertional Achilles Tendinitis: This type impacts the lower part of the tendon where it attaches to the heel bone. While it can affect anyone, including non-active individuals, it is most common in those who overuse the tendon, like long-distance runners.
Symptoms
Achilles tendinitis primarily affects the back of the lower leg, just above the heel, and can cause discomfort during and after physical activity. Common symptoms include:
- Pain in the Heel and Ankle: Pain along the Achilles tendon, especially at the back of the heel, often worsens with activity.
- Stiffness: Tendon stiffness, particularly noticeable in the morning, may improve as the day progresses.
Swelling: The area around the Achilles tendon may become swollen, with the swelling worsening throughout the day or during activity. - Leg Weakness: You might feel weakness in your leg, particularly when climbing stairs or walking uphill.
- Thickened Tendon: The Achilles tendon may thicken over time due to inflammation or degeneration.
- Bone Spurs: Bone spurs can form in cases of insertional tendinitis, where the tendon connects to the heel.
- Increased Pain with Shoes: Wearing shoes may cause discomfort or pain at the back of the heel.
Symptoms are typically worse after physical activity or the day after exercising, and pain may intensify when climbing stairs. If you experience a sudden “pop” in the back of your calf or heel, it could indicate a tendon tear, and medical attention should be sought immediately.
Who Is at Risk for Achilles Tendinitis?
Achilles tendinitis is a common injury, particularly for those involved in sports or activities that put stress on the feet and ankles. High-risk groups include:
- Athletes: Individuals who play sports that involve sudden starts and stops, like tennis, basketball, or soccer.
- Runners and Dancers: These activities can place repetitive stress on the Achilles tendon, leading to injury.
- Laborers: Jobs that require standing or walking for extended periods can strain the Achilles tendon.
- Weekend Warriors: People who participate in sports or physical activity infrequently are more likely to develop Achilles tendinitis, as their bodies may not be accustomed to the stress.
Certain anatomical factors can also increase your risk, such as:
- Tight or Weak Calf Muscles: These can put extra strain on the Achilles tendon.
- Bone Spurs: Extra bone growth on the heel can irritate the Achilles tendon.
- Flat Feet or Overpronation: Feet with flat arches or ankles that roll inward when walking can cause additional strain on the tendon.
Complications of Achilles Tendinitis
If left untreated, Achilles tendinitis can lead to more severe issues, including:
Achilles Tendinosis: The tendon begins to break down or degenerate over time.
Achilles Tendon Rupture: In severe cases, the tendon can tear or separate from the heel bone, often requiring surgical intervention.
Management and Treatment of Achilles Tendinitis
Achilles tendinitis can be managed through both nonsurgical and surgical methods. In most cases, nonsurgical treatments are effective, although recovery may take several months.
Nonsurgical Treatment Options
1. RICE Method (Rest, Ice, Compression, Elevation):
- Rest: Avoid activities that stress the tendon, and switch to low-impact exercises like swimming.
- Ice: Apply ice for up to 20 minutes to reduce pain and swelling.
- Compression: Use athletic wraps to apply pressure to the tendon.
- Elevation: Keep the foot elevated to reduce swelling.
2. Footwear Modifications:
- Wear supportive shoes or orthotics.
- Consider heel lifts or custom orthotics to reduce strain on the tendon.
3. Physical Therapy:
- Stretching and strengthening exercises (like calf stretches and eccentric heel drops) are crucial for recovery.
- Night splints can help maintain tendon flexibility while sleeping.
4. Shockwave Therapy:
- This non-invasive therapy uses sound waves to reduce pain and promote healing.
5. Medications:
- NSAIDs (e.g., ibuprofen) can help with pain and inflammation, but prolonged use should be monitored by a healthcare provider.
6. Other Treatments:
- Brisement: Injecting anesthetic to break up scar tissue.
- PRP Injections: Platelet-rich plasma injections may promote tendon healing.
Surgical Treatment Options
If nonsurgical methods fail after six months, surgery may be necessary. Surgical options include:
1. Debridement and Repair:
- The surgeon removes damaged tendon tissue and stitches the remaining healthy tendon.
2. Gastrocnemius Recession:
- Lengthening the calf muscles to reduce stress on the Achilles tendon.
3. Tendon Transfer:
- For severe cases where over 50% of the tendon is damaged, the tendon is replaced with another tendon from the foot.
4. Hydrocision TenJet®:
- A minimally invasive procedure that uses saline to break up scar tissue.
Prevention Strategies:
To mitigate Achilles tendinitis risk:
- Gradually increase physical activity
- Wear proper, supportive footwear
- Daily stretching routines
- Strengthen calf muscles
- Incorporate low-impact activities into training
If heel pain persists or Achilles tendinitis is suspected, consult a healthcare professional for tailored guidance and treatment options.
Conclusion:
Achilles tendinitis is a common ailment, but with comprehensive care, including physiotherapy and osteopathy, individuals can effectively manage this condition and regain their mobility and comfort. If persistent heel pain or Achilles tendinitis is suspected, it is imperative to consult a healthcare professional who can provide personalized guidance and a tailored treatment plan.