Scoliosis – What It Is, Types, Symptoms
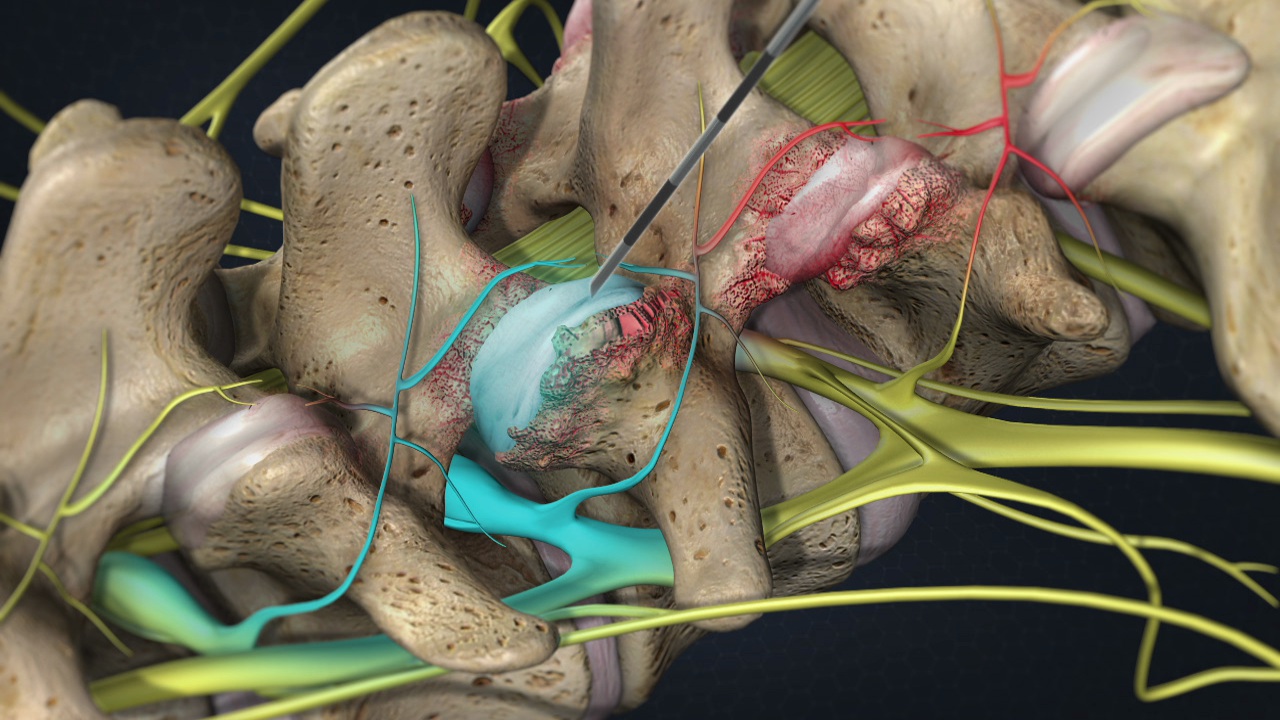
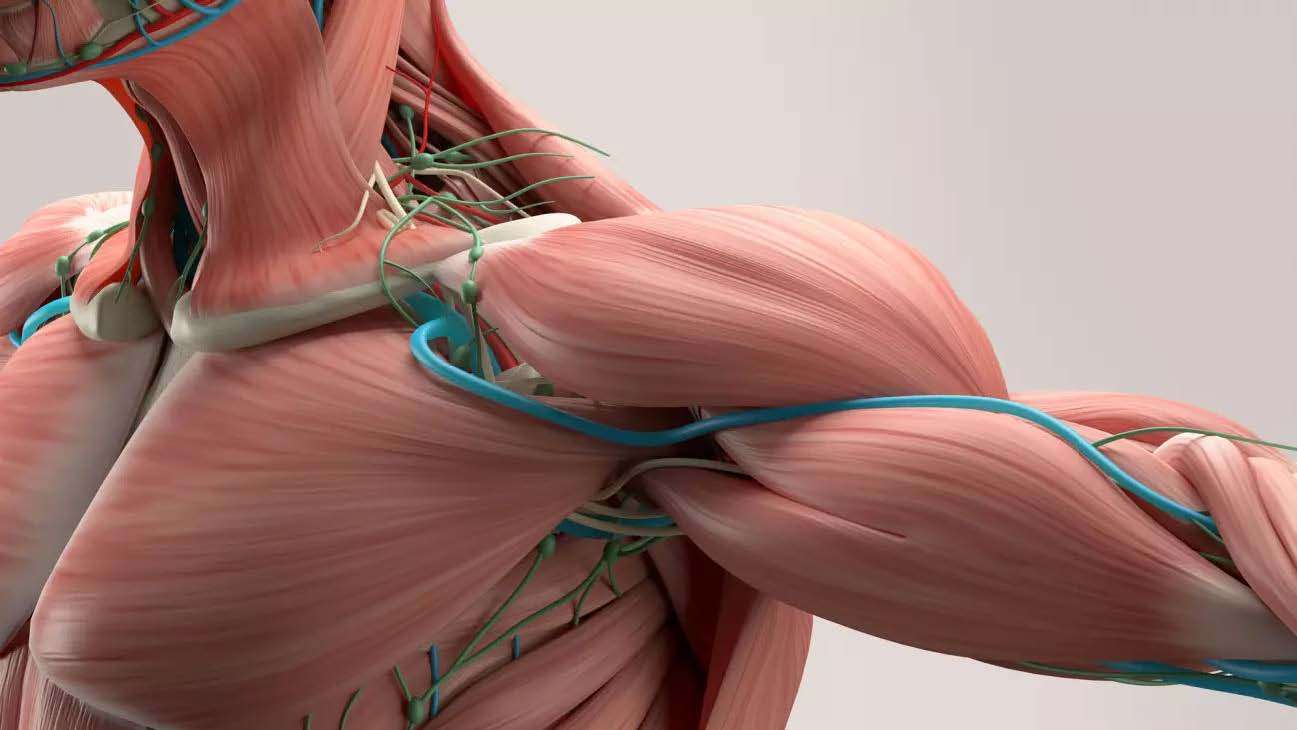
What is scoliosis? Scoliosis is an abnormal side-to-side curvature of the spine, differing from the spine’s natural forward and backward curve. Typically diagnosed during adolescence, scoliosis is usually mild and asymptomatic but can occasionally lead to back pain and abnormal posture. Treatment options include physical therapy, braces, and surgery. Types of Scoliosis There are three main types of scoliosis: Idiopathic Scoliosis: The most common type, with an unknown cause, though it often runs in families and has a genetic link. Congenital Scoliosis: A rare spine abnormality detected at birth, caused by vertebrae not forming correctly during embryonic development. Neuromuscular Scoliosis: Resulting from abnormalities in muscles and nerves, often associated with neurological or muscular conditions like cerebral palsy, spina bifida, or muscular dystrophy. Scoliosis diagnosed during adulthood is often referred to as adult-onset scoliosis or degenerative scoliosis. This can occur due to the weakening of disks and joints or loss of bone density (osteoporosis), leading to increased symptoms over time. Symptoms and Causes What are the Symptoms of Scoliosis? Scoliosis usually doesn’t cause symptoms, but when present, they may include: Back pain Difficulty standing upright Core muscle weakness Leg pain, numbness, or weakness What are the Signs of Scoliosis? Signs of scoliosis may include: Uneven shoulders Shoulder blades that stick out Head that doesn’t center above the pelvis Uneven waist Elevated hips Constant leaning to one side Uneven leg length If you notice any of these signs, contact a healthcare provider for a screening. Over time, you may notice height loss and uneven alignment of the pelvis and hips. What Part of the Spine Does Scoliosis Affect? Scoliosis can affect any part of the spine, with differences according to age: Adolescents: Most cases occur in the thoracic spine (rib cage) area. Adults: The main concern is in the lumbar or lower spine, which is most susceptible to changes seen with aging or degeneration, increasing symptoms like pain. Diagnosis and Tests The first step in diagnosing scoliosis is a screening, typically performed during pediatric wellness visits or school check-ups. During a screening, a provider will ask the patient to: Remove their shirt to see the back. Stand up straight. Bend forward (as if touching their toes). A screening helps the provider assess posture, alignment, and spinal curvatures. If scoliosis is suspected, further imaging tests like X-rays, MRI, or CT scans may be ordered. How is Scoliosis Diagnosed? A healthcare provider will diagnose scoliosis after a physical exam, which includes standing straight and bending forward to touch the toes. The provider will examine the back, check the shape of the spine, and assess nerve function by testing reflexes and muscle strength. Before suggesting a treatment plan, the provider will ask about: Medical history and family medical history The date of initial symptom onset or screening Any bowel, bladder, or motor symptoms, which may indicate serious nerve damage or pressure caused by scoliosis If necessary, imaging tests like X-rays, MRI, or CT scans will be ordered to provide a detailed picture of the spine and determine the degree of curvature. I am text block. Click edit button to change this text. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo. How is Scoliosis Measured? A healthcare provider measures the spinal curve in degrees, categorizing the severity: No scoliosis diagnosis: Less than 10 degrees Mild scoliosis: Between 10 to 24 degrees Moderate scoliosis: Between 25 to 39 degrees Severe scoliosis: More than 40 degrees Providers use a device called a scoliometer to measure the curve and may also order X-rays for a more accurate assessment. Management and Treatment How is Scoliosis Treated? Treatment for scoliosis isn’t necessary for all cases. If recommended, treatment aims to relieve symptoms and prevent curve progression. Options include: Nonsurgical Treatment: Regular monitoring, pain relievers, core strengthening exercises, wearing a back brace, and managing underlying conditions. Surgical Treatment: Recommended for severe cases unresponsive to conservative treatment, including spinal fusion or expandable rod insertion to stabilize and support the spine. Conclusion Understanding scoliosis—from its types and causes to symptoms, diagnosis, and treatment options—is crucial for effective management. Early detection through regular screenings and appropriate treatment can help manage symptoms and improve the quality of life for those affected by scoliosis.